You trust the little pills that keep your blood pressure down, ease your arthritis pain, or knock out that nagging heartburn. You take them exactly as directed. Yet every single day, thousands of Americans are rushed to dialysis because the medicines meant to help them slowly destroyed their kidneys instead.
The scariest part? Most people feel perfectly fine—until the lab results come back and it’s too late. Protein starts spilling into the urine. Creatinine climbs. And suddenly “stage 3” becomes “stage 5” almost overnight.
If you’re over 50, already have even slightly elevated blood pressure, diabetes, or a trace of protein in your urine, you cannot afford to skip this list. One or more of these common drugs might be the hidden reason your kidney function is slipping—despite “everything else looking good.”
Why Your Kidneys Are More Vulnerable Than You Think
Your kidneys filter about 50 gallons of blood every single day. They’re tough—but they’re not invincible. Certain medications force them to work overtime, cause direct injury to delicate filtering tubes, or shrink the tiny blood vessels that keep them alive.
The damage is usually silent. You won’t feel pain. You won’t see warning signs until 60–70% of kidney function is already gone. That’s why nephrologists call these drugs “the perfect assassins.”
The 10 Common Medications Nephrologists Wish More Patients Knew About
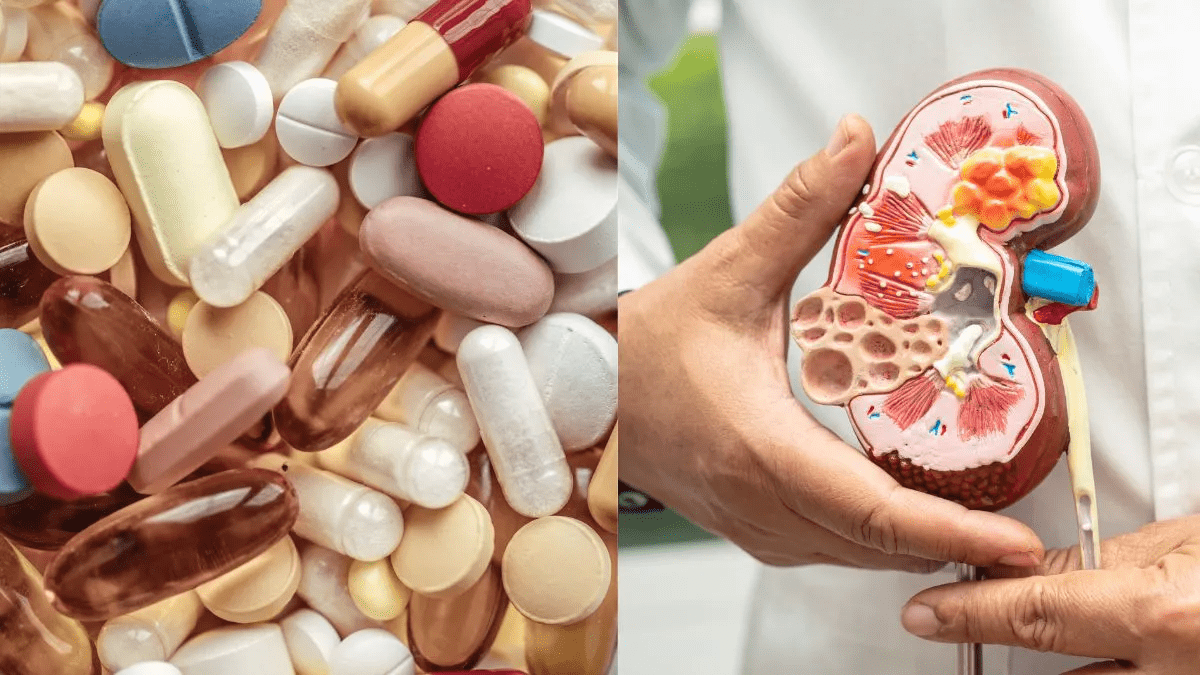
- Ibuprofen, Naproxen, and Other Over-the-Counter NSAIDs You pop them for back pain, headaches, or weekend warrior aches. Long-term or high-dose use can drop kidney blood flow by up to 50% in hours. Studies show regular NSAID users have triple the risk of sudden kidney injury.
- Heartburn Pills: Proton Pump Inhibitors (PPIs) – Omeprazole, Esomeprazole, Lansoprazole Over 15 million Americans take these daily. A 2023 JAMA study linked PPI use longer than 90 days with a 20–50% higher risk of chronic kidney disease. Many patients notice rising creatinine only after years of “harmless” purple capsules.
- Certain Blood Pressure Meds: ACE Inhibitors & ARBs (When Combined with NSAIDs or Diuretics) Yes—the very drugs that protect kidneys in most people can backfire when combined with NSAIDs or dehydration. The infamous “triple whammy” can crash kidney function in as little as one week.
- Some Antibiotics: Gentamicin, Vancomycin, and Older Penicillins One short course in the hospital can cause permanent damage in up to 30% of patients—especially if you’re older or already have reduced kidney function.
- Contrast Dye Used in CT Scans and Angiograms A single scan with iodine contrast can trigger kidney injury in 1 out of 5 high-risk patients. Doctors call it “contrast-induced nephropathy,” but patients just hear “your kidneys may never recover.”
- Lithium (Still Widely Used for Bipolar Disorder) Up to 40% of long-term lithium users develop chronic kidney disease. The damage often shows up 10–20 years after starting the medication.
- Chemotherapy Drugs: Cisplatin and Others Powerful cancer fighters that can destroy kidney tubules in weeks. Many survivors trade cancer for lifelong dialysis.
- Weight-Loss and Diabetes Drug: Semaglutide (Ozempic, Wegovy) – Emerging Reports Early data and case reports show rare but severe acute kidney injury, especially in people who get dehydrated from vomiting or diarrhea.
- High-Dose Vitamin C IV Therapy (Popular in Wellness Clinics) Mega-doses can crystallize in the kidneys and cause oxalate stones or sudden failure. Yes—even “natural” treatments can backfire.
- The Silent Leader: Long-Term, High-Dose Tylenol (Acetaminophen) Mixed with Alcohol Most people think acetaminophen is “safe for kidneys.” It’s not when combined with even occasional alcohol or taken daily for chronic pain. It’s now one of the top causes of acute liver AND kidney failure in the U.S.
How to Tell If Your Medications Are Already Hurting Your Kidneys
| Early Red Flag | What It Might Mean |
|---|---|
| Foamy or bubbly urine | Protein leaking through damaged filters |
| Swelling in ankles or hands | Kidneys not removing fluid properly |
| Fatigue that’s worse than usual | Toxins building up in blood |
| Lower back pain on both sides | Possible inflammation around the kidneys |
| Creatinine rising slowly | The only lab test that catches it early |
| Urine color suddenly dark | Dehydration + medication stress |
What You Can Do Right Now – Without Stopping Any Medication Cold Turkey
- Ask your doctor or pharmacist for your latest eGFR and urine albumin-to-creatinine ratio. If eGFR is under 60 or protein is spilling, red flags are already up.
- Bring a complete list (including supplements and OTC meds) to every appointment.
- Never take ibuprofen or Aleve on the same day as your blood pressure pill without checking first.
- Stay aggressively hydrated—aim for pale yellow urine all day.
- Request the lowest effective dose and frequent monitoring if you must stay on a high-risk drug.
- Consider safer alternatives: topical NSAIDs, acetaminophen (in strict moderation), physical therapy, or turmeric/ginger for inflammation.
The Bottom Line You Need to Hear Today
Your kidneys don’t come with backup batteries. Once the damage passes a certain point, there’s no rewind button—only dialysis or transplant.
The good news? In many cases, simply switching or lowering the dose of one medication can halt the decline and even let kidneys partially heal.
Don’t wait for the “you’re in kidney failure” conversation that happens far too often in emergency rooms.
Take this article with you to your next appointment. Ask the hard questions. Your kidneys will thank you—and you might just save the only pair you’ll ever have.
This article is for educational purposes only and is not medical advice. Always consult your physician or nephrologist before making any changes to prescribed medications.