Imagine noticing persistent foamy urine in the toilet—those stubborn bubbles that linger longer than a quick flush should clear—accompanied by vague fatigue, mild swelling around the ankles, or a nagging sense of unease in your lower back. You’ve probably come across alarming posts claiming a “natural secret” can slash creatinine levels and rescue kidneys from damage in just 19 hours, often with dramatic before-and-after urine photos or a concerned older man clutching his side. While foamy urine can signal protein leakage (proteinuria) and elevated creatinine often points to reduced kidney filtration, no single remedy or food transforms kidney health that rapidly. Dramatic short-term fixes lack scientific backing and can mislead people delaying proper care. For many over 45 facing creeping creatinine trends, subtle lifestyle and dietary shifts offer realistic, evidence-based support to ease kidney burden over weeks to months. Curious about what actually helps? Let’s explore the grounded steps that matter.
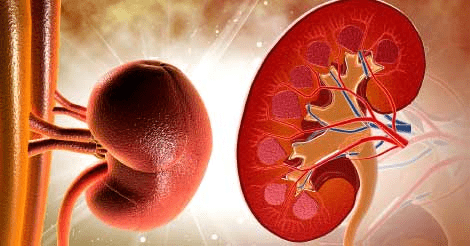
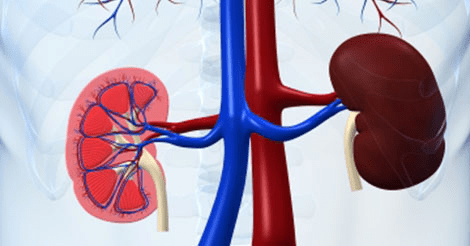
Kidney concerns build quietly: high blood pressure strains filters, uncontrolled diabetes damages vessels, dehydration concentrates waste, or excess protein intake overloads processing. Foamy urine often stems from protein slipping through damaged glomeruli, while high creatinine reflects muscles breaking down creatine into waste that kidneys struggle to clear. These issues link to broader risks like heart strain or fatigue. Research emphasizes managing root causes—pressure, sugar, hydration—over miracle cures.
The appeal of quick “secrets” is understandable amid worry, but reputable sources like the National Kidney Foundation and Mayo Clinic stress consistent habits prevent progression far better than unproven recipes. No herb, juice, or seed drops creatinine dramatically in hours; temporary dips (like from heavy water intake) don’t fix underlying function. Let’s build anticipation: What small, sustainable changes show real promise?
Hydration: The Foundation of Kidney Flush
Picture starting your day with steady sips of plain water, feeling that gentle flow supporting your system’s natural clearance. Dehydration concentrates urine, potentially worsening foaminess and elevating creatinine temporarily. Evidence shows adequate hydration (around 1.5–2 liters daily for most, adjusted for health) helps kidneys dilute and excrete waste more efficiently.
Many notice clearer, less concentrated urine after prioritizing fluids—the refreshing sensation becomes a mindful cue. For those without fluid restrictions, this simple step aids overall filtration. But hydration pairs best with diet tweaks—next up, protein moderation.
Moderating Protein Intake: Easing the Load
Ever feel weighed down after heavy meat meals? High animal protein (especially red/processed) increases creatinine production as the body metabolizes creatine. Studies link lower protein diets (especially plant-focused) to reduced creatinine and slower CKD progression in some cases.
Think of shifting toward lentils, beans, tofu, or egg whites—satisfying yet gentler. Research suggests plant-based patterns lessen hyperfiltration strain on kidneys. Users often report steadier energy without extreme restriction. Fair question: “Won’t I lack protein?” Balance with variety—consult a dietitian for personalized targets. Fiber steps in next for added support.
Boosting Fiber: Gentle Detox Aid
Bloating or sluggish digestion alongside kidney worries? Fiber-rich foods like oats, berries, apples, and non-starchy veggies (cauliflower, bell peppers) may help bind waste and promote regularity, indirectly easing kidney burden. Some evidence ties higher fiber to modest creatinine benefits via better gut-kidney axis.
Imagine adding a handful of berries or steamed veggies daily—the natural sweetness or crunch makes it enjoyable. Fiber slows absorption and supports blood sugar stability, crucial since diabetes accelerates kidney issues. Intriguing, right? Sodium control amplifies these gains.
Cutting Sodium: Protecting Pressure and Balance
Salt creeps in everywhere, raising blood pressure that damages kidney vessels over time. Lowering sodium (aim under 2,300 mg/day, ideally 1,500 for kidney concerns) helps maintain fluid balance and reduces strain.
Many feel less puffy or tight after swapping processed foods for home-cooked with herbs/lemon. Evidence shows sodium reduction supports better filtration and may stabilize creatinine indirectly. But wait—lifestyle factors tie it together.
Movement and Pressure Management: Daily Resilience
Sedentary days compound risks; moderate activity (walking, swimming) improves circulation, controls weight, and helps regulate blood pressure—key for kidney protection. Studies highlight how consistent movement slows progression in early CKD.
Picture a brisk 20–30 minute walk—the fresh air and rhythm lift mood while supporting filtration. Combine with stress reduction (deep breathing, sleep) for compounded benefits. The overall shift emerges next.
The Cumulative Kidney Support Shift
But here’s the real potential: Weaving hydration, moderated protein, fiber focus, low sodium, and movement might gradually ease creatinine trends, reduce foaminess (if proteinuria-related), and foster steadier function. No overnight transformation—science points to months of consistency for noticeable lab shifts—but these habits empower long-term resilience.
Comparing Kidney-Supportive Habits and Their Potential Impact
| Habit | Key Mechanism | Evidence-Based Potential Benefit |
|---|---|---|
| Adequate Hydration | Dilutes waste, aids excretion | May temporarily lower concentrated creatinine; supports filtration |
| Moderate/Lower Protein | Reduces creatinine production | Plant-focused diets linked to slower progression, modest reductions |
| High Fiber Intake | Binds waste, gut-kidney support | Indirect help via blood sugar/inflammation control |
| Low Sodium | Lowers blood pressure strain | Helps preserve function, reduces swelling/foam risk |
| Regular Movement | Improves circulation, BP control | Slows decline, enhances overall resilience |
- Focus on whole foods low in processed additives.
- Prioritize fruits/veggies for antioxidants.
- Avoid self-prescribed “detox” herbs—many risk kidney harm.
Safe Ways to Start Supporting Your Kidneys
Begin gradually: Track water intake, swap one high-protein meal for plant-based, cut salty snacks.
- Drink water steadily—add lemon for flavor if plain bores you.
- Choose home-cooked over processed.
- Monitor urine changes mindfully.
Practical Guidance Table
| Aspect | Suggestion | Caution/Note |
|---|---|---|
| Daily Water | 1.5–2L (or as doctor advises) | Avoid excess if fluid-restricted |
| Protein | Moderate; prefer plant sources | Get personalized limits from nephrologist |
| Sodium | <2,300 mg/day | Read labels; use herbs instead of salt |
| Monitoring | Note urine, energy, swelling | See doctor for persistent foam/high creatinine |
| When to Seek Help | Foamy urine ongoing, fatigue, swelling | Urgent if blood in urine or severe pain |
Always consult your healthcare provider before changes—especially with diagnosed CKD, meds, or symptoms. Foamy urine warrants urinalysis; high creatinine needs professional evaluation. These steps complement, never replace, medical care.
You might think, “Can this really help me?” Effects vary by cause and stage—many report steadier labs and comfort with consistency, but it’s no quick fix.
What if these habits lighten your kidney worries? Recap: hydration for clearance, protein moderation to reduce load, fiber/sodium tweaks for balance, movement for resilience. Start one change today—observe mindfully. P.S. Surprising note: Persistent foamy urine often signals treatable proteinuria—early checkups make a big difference.
Share your kidney health insights below—any surprises?
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.