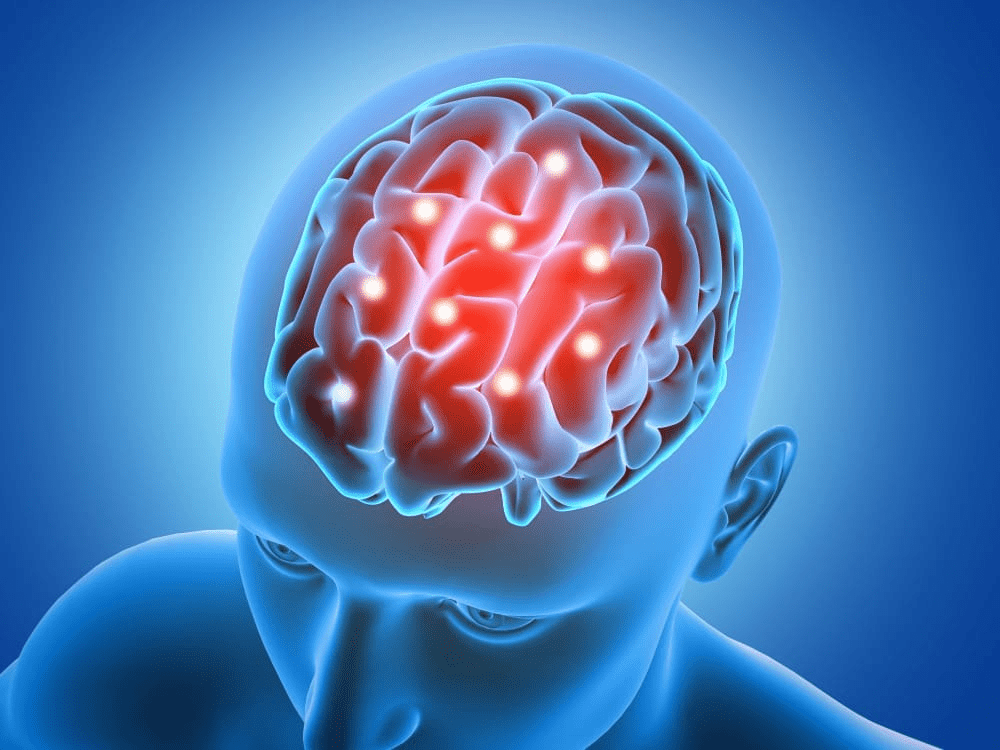
Picture this: You’re reaching for your morning coffee, but your hand feels oddly clumsy, like it doesn’t quite belong to you. Or you stand up from a chair and notice a sudden wobble in one leg that wasn’t there yesterday. These subtle changes can feel like “just getting older”—fatigue, a bad night’s sleep, or arthritis acting up. But for many seniors over 60, they may signal something far more serious: a lacunar stroke. These small, deep-brain events account for about 20–25% of all ischemic strokes and often fly under the radar because symptoms are mild and don’t scream “emergency” like larger strokes do.
Lacunar strokes happen when tiny penetrating arteries deep in the brain get blocked, creating small infarcts (lacunes) in areas controlling movement, sensation, and coordination. Unlike big cortical strokes, they rarely cause dramatic confusion, severe aphasia, or one-sided paralysis that everyone recognizes. Instead, signs creep in quietly—easy to dismiss as normal aging. Yet early recognition matters hugely: acting fast can limit damage, prevent recurrence, and improve long-term outcomes. The good news? Knowing these patterns empowers you to spot trouble sooner.
The Hidden Danger: Why Lacunar Strokes Get Overlooked in Seniors
Lacunar strokes are linked to chronic conditions common after 60—high blood pressure (the biggest risk factor), diabetes, high cholesterol, and smoking—which damage small vessels over years. Many are “silent” or produce only fleeting symptoms, yet repeated ones raise risks for vascular dementia, mobility issues, and future major strokes. Studies show up to 20–50% of older adults have asymptomatic lacunes on imaging, but when symptoms appear, they’re often brushed off. The classic BE FAST stroke signs (Balance issues, Eyes/vision changes, Face drooping, Arm weakness, Speech difficulty, Time to call emergency) still apply, but lacunar events emphasize subtler motor, sensory, or coordination changes without obvious cortical signs like neglect or severe language loss.
Countdown: 7 Key Warning Signs of Lacunar Stroke (Many Seniors Miss #4)
Let’s count down seven signs backed by clinical research, starting with the most common. These often appear suddenly or progress gradually (“stuttering” over hours/days).
- Sudden Clumsiness or Ataxia on One Side One limb (arm or leg) feels uncoordinated or unsteady—tripping more, dropping things, or feeling “drunk” on one side. This ataxic hemiparesis syndrome stems from damage in motor pathways or cerebellum connections. Often blamed on age-related balance decline.
- Pure Sensory Changes – Numbness or Tingling on One Side Unilateral numbness, pins-and-needles, or altered sensation (touch, temperature, pain) affecting face, arm, and leg without weakness. This pure sensory stroke hits thalamic areas; seniors might attribute it to neuropathy or poor circulation.
- Dysarthria-Clumsy Hand Syndrome Slurred speech combined with hand clumsiness—trouble with fine tasks like buttoning shirts or writing. Facial weakness may be mild. This common syndrome gets dismissed as fatigue or dental issues.
- Subtle Weakness or Drooping (The One Everyone Overlooks) Mild one-sided weakness or paralysis in the face, arm, or leg—often equal across them—without dramatic droop or total loss of function. Pure motor hemiparesis (most frequent, ~45% of cases) feels like “my leg just gave out” or “my arm feels heavy.” Seniors overlook it as arthritis, muscle strain, or “old age weakness”—yet it’s a classic red flag. No sensory loss or speech issues make it sneakier.
- Sudden Dizziness, Vertigo, or Balance Loss Unexplained spinning, swaying, or imbalance without full spinning vertigo. Often paired with nausea. Brainstem or cerebellar involvement; many blame inner-ear problems or low blood pressure.
- Difficulty Walking or Gait Changes Sudden trouble walking straight, shuffling, or leg heaviness—without obvious pain. Ataxic or hemiparetic patterns emerge; seniors think “I’m just stiff today.”
- Sudden Severe Headache or Unusual Head Pressure A “thunderclap” or unusually intense headache with no clear cause—sometimes the only sign. Can signal vessel issues; often dismissed as tension or migraine.
But wait—there’s one more critical point: symptoms can fluctuate or resolve quickly (like a TIA), yet still warn of underlying vessel damage. Multiple small events build risk for cognitive decline or bigger strokes.
Real Stories That Could Sound Familiar
Meet Robert, 72, who ignored “clumsy” hand episodes for weeks—blamed it on arthritis. A mild arm weakness finally prompted a check-up; imaging showed multiple lacunes. Early intervention with blood pressure control prevented worse outcomes. “I thought it was nothing—glad I didn’t wait,” he shared.
Or Susan, 68, who dismissed sudden leg numbness as sitting too long. When dizziness hit, she sought help—catching lacunar changes early allowed lifestyle tweaks and meds to stabilize things.
Have any of these felt vaguely familiar, even if mild?
Quick Reference: Classic Lacunar Syndromes vs. Everyday Complaints
| Syndrome | Key Signs | Why Overlooked in Seniors |
|---|---|---|
| Pure Motor Hemiparesis | Weakness/paralysis one side (face/arm/leg equal) | “Just weak from age/arthritis” |
| Pure Sensory Stroke | Numbness/tingling one side | “Neuropathy or poor circulation” |
| Ataxic Hemiparesis | Clumsiness + weakness one side | “Balance issues from getting older” |
| Dysarthria-Clumsy Hand | Slurred speech + hand clumsiness | “Tired voice or stiff fingers” |
| Mixed Sensorimotor | Weakness + numbness one side | “Combo of old injuries” |
Safety and Next Steps
If any sign appears suddenly—even if mild—use BE FAST and call emergency services immediately. Time saves brain tissue. For seniors:
- Monitor blood pressure regularly (target <130/80 often recommended).
- Manage diabetes, cholesterol, and quit smoking.
- Stay active, eat heart-healthy, and consider low-dose aspirin if advised.
You know your body best. A subtle change isn’t always “normal aging”—trust your instincts and get checked.
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Stroke symptoms require immediate emergency care—call your local emergency number right away if you suspect a stroke. Always consult your healthcare provider for personalized guidance, especially with risk factors like hypertension or diabetes. Individual experiences vary.






