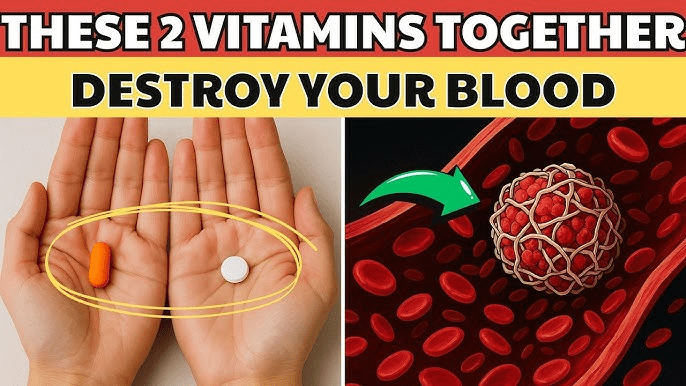
Imagine reaching for your daily supplements, feeling proactive about your health, only to unknowingly create a hidden conflict inside your body. For seniors over 60, this happens more often than you think. Many take multiple vitamins and minerals to support bones, immunity, energy, or heart health—yet certain popular combinations can interfere with absorption, reduce benefits, or even heighten risks like bleeding or nutrient deficiencies.

The stakes are higher after 60: slower metabolism, common medications, and age-related changes make interactions more impactful. Research from dietitians and health organizations warns that poor timing or pairing can turn helpful supplements into problems. What if two common ones you’re taking right now are quietly working against each other?
The tension builds: Which two stand out as especially risky for seniors? Let’s uncover the top dangerous duo many experts highlight, plus why it matters and safer ways forward.
Why Supplement Interactions Hit Seniors Harder
Aging bodies absorb nutrients differently—kidneys and liver process slower, and polypharmacy (multiple meds) adds complexity. Common supplements like calcium for bones or iron for energy often get combined without realizing they compete.
Evidence shows minerals like calcium, iron, zinc, and magnesium share absorption pathways in the gut. Taking them together reduces how much your body actually uses—potentially leading to deficiencies despite supplementation.
You might think, “My multivitamin has everything together—it’s fine.” Many multis use lower doses, but separate high-dose supplements amplify issues. Studies indicate seniors face higher risks from these clashes, especially with bone, blood, or fatigue concerns.
But the real danger? One standout pair tops lists for absorption sabotage.
The Risky Duo: Calcium and Iron Supplements
Picture calcium building strong bones while iron keeps energy steady—great on their own, but disastrous together. Calcium blocks iron absorption in the intestines, sometimes cutting uptake by 50% or more when taken at the same time.
Seniors often take calcium for osteoporosis prevention and iron for anemia or low energy—common after 60. Research confirms calcium (especially doses over 300-500mg) significantly reduces non-heme iron absorption from supplements or food.
One review found short-term studies show clear interference, while long-term effects vary but still warrant caution. For older adults, untreated low iron risks fatigue, weakness, falls, and heart strain—exactly what you don’t need.
Experts recommend separating them by at least 2 hours—ideally more. Take iron on an empty stomach for best absorption, calcium with meals.
But is this the only concern? Many sources flag a second high-risk pair for seniors.

Another Dangerous Combination: High-Dose Vitamin E and Blood Thinners (or Similar Supplements)
Envision vitamin E supporting skin, heart, or immunity—popular among seniors. Yet high doses (over 400 IU daily) can enhance blood-thinning effects, especially if you’re on warfarin, aspirin, or other anticoagulants.
Vitamin E interferes with clotting factors and platelet function, potentially increasing bleeding risks like bruising, nosebleeds, or serious internal issues. Studies link higher vitamin E levels to more bleeding events in those on oral anticoagulants.
Seniors face elevated stroke or clot risks, so many take blood thinners—making this combo particularly hazardous. Even without meds, combining vitamin E with other blood-thinners like fish oil or garlic amplifies concerns.
Doctors advise caution or avoidance—check levels and consult before mixing.
These two pairings—calcium/iron for absorption loss and vitamin E with blood thinners for bleeding risk—top warnings for seniors.

Safer Ways to Take Supplements Without the Danger
Space them out: Iron in the morning empty stomach, calcium midday or evening with food.
Get tested: Blood work reveals actual needs—avoid guessing.
Choose food first: Leafy greens for calcium, lean meats/beans for iron—less interaction worry.
Talk to your doctor or pharmacist: They review your full list, including meds.
| Combination | Main Risk for Seniors | Why It Happens | Safer Timing/Alternative |
|---|---|---|---|
| Calcium + Iron | Reduced iron absorption (up to 50% loss) | Compete for gut transporters | Separate by 2+ hours; iron empty, calcium with meals |
| High-Dose Vitamin E + Blood Thinners (e.g., warfarin) | Increased bleeding risk | Vitamin E affects clotting | Avoid high doses; monitor INR if on anticoagulants |
This comparison highlights why separation or caution matters.
| Step | Action | Timing Suggestion | Pro Tip |
|---|---|---|---|
| 1 | List all supplements/meds | Review weekly | Include herbals like garlic |
| 2 | Space mineral doses | 2-4 hours apart | Iron morning, calcium afternoon/evening |
| 3 | Check with provider | Before any change | Bring bottles to appointments |
| 4 | Prioritize food sources | Daily meals | Spinach for iron/calcium balance |
| 5 | Monitor symptoms | Ongoing | Fatigue? Bruising? Report promptly |

These steps keep benefits high while risks low.
Have you checked if your routine includes risky pairs? Small tweaks could protect your health.
In summary, seniors should avoid taking calcium and iron together due to absorption interference, and high-dose vitamin E with blood thinners due to bleeding risks. These combinations, common after 60, can undermine benefits or cause harm—yet spacing doses, testing needs, and consulting pros keep things safe.
Review your supplements today—discuss with your doctor. Knowledge empowers healthier aging.
P.S. A simple blood test often reveals if you’re truly deficient—preventing unnecessary risks from over-supplementation.
This article is for informational purposes only and is not a substitute for professional medical advice—consult your healthcare provider for personalized guidance.