You wake up, check your blood pressure monitor, and see those numbers creeping higher again. The frustration builds— you’ve cut back on salt at the table, yet the readings won’t budge. What if the real culprits aren’t the shaker, but everyday foods hiding massive amounts of sodium, saturated fats, or sugars?
High blood pressure, or hypertension, affects millions and quietly raises risks for heart disease, stroke, and kidney issues. The American Heart Association notes most adults should aim for no more than 2,300 mg of sodium daily—ideally 1,500 mg if you have hypertension. Yet average intake often exceeds 3,400 mg, largely from processed and restaurant foods.
Research, including the DASH diet studies, shows slashing sodium and unhealthy fats can lower blood pressure noticeably in weeks. But spotting the offenders takes vigilance. Have you scanned labels on your favorites lately? Let’s uncover seven common foods that research suggests may contribute to higher readings when eaten regularly—and simple ways to sidestep them.
The Silent Impact of Hidden Ingredients
Sodium causes fluid retention, forcing your heart to pump harder. Saturated fats and added sugars add weight and inflammation, compounding the strain. These elements often team up in convenient foods, making moderation tricky.
Many people feel the effects subtly—headaches, fatigue, or swelling—without connecting them to diet. But consistent choices matter. Studies link high-sodium patterns to sustained hypertension. Ready to identify the top offenders?
7 Foods Often Linked to Higher Blood Pressure
These items frequently top lists from sources like the American Heart Association, Mayo Clinic, and WebMD for their sodium, fat, or sugar content. Limiting them supports better control.
1. Processed Meats (Bacon, Sausages, Deli Meats, Hot Dogs) That crispy bacon strip or lunchtime sandwich feels comforting. Yet a few slices can pack 500–1,000 mg sodium, plus saturated fats and preservatives. Research associates regular processed meat intake with elevated blood pressure through inflammation and vessel strain. One analysis tied higher consumption to increased hypertension odds.

2. Canned Soups and Broths Warm and quick on a chilly day, but a single can often exceeds 800–1,200 mg sodium—half or more of your daily limit. Even “healthy” varieties hide added salt for flavor. Frequent use contributes to cumulative overload, making blood pressure harder to manage.
3. Frozen or Restaurant Pizzas The cheesy pull and savory sauce tempt many. A slice or small personal pizza delivers 700–1,500 mg sodium from dough, cheese, sauce, and toppings. Processed versions add saturated fats. Studies highlight pizza as a top sodium source in American diets, linked to poorer cardiovascular profiles.
4. Salty Snacks (Chips, Pretzels, Crackers) Crunchy handfuls satisfy cravings fast. A small serving packs 150–300 mg sodium, and it’s easy to overeat. Regular munching adds up quickly, pushing intake beyond recommendations and potentially raising pressure over time.
5. Cheese (Especially Processed or Hard Varieties) Melted on burgers or grated over pasta, cheese adds richness. But many types—American, cheddar, cottage—contain 300–500 mg sodium per ounce or half-cup. Saturated fats compound concerns. Lower-sodium options like Swiss exist, but moderation helps.
6. Condiments and Sauces (Soy Sauce, Ketchup, Salad Dressings) A drizzle seems harmless. Yet soy sauce can hit 900 mg per tablespoon, ketchup and dressings add hundreds more. These sneaky additions turn low-sodium meals high quickly. Research shows condiments contribute significantly to daily totals.
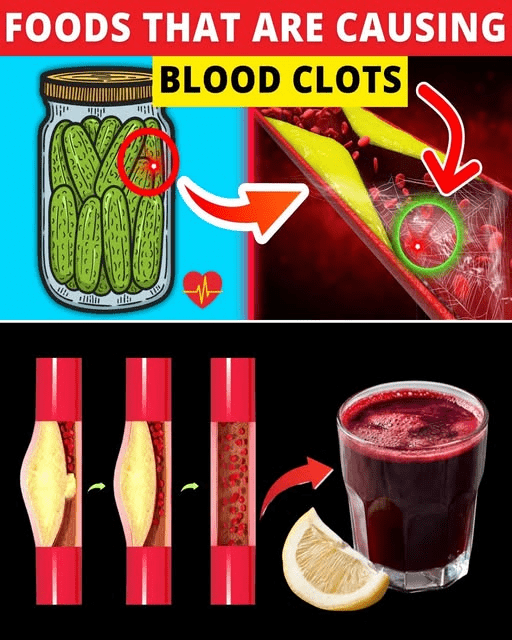
7. Pickled or Fermented Foods (Pickles, Olives, Sauerkraut) Tangy and flavorful, but brining means high sodium—often 500–900 mg per serving. While some offer probiotics, excess salt outweighs benefits for blood pressure management in many cases.
But here’s the hopeful part—avoiding these opens space for protective foods that actively support healthier levels.

Smarter Swaps for Everyday Wins
Focus on fresh, whole options rich in potassium, which counters sodium. Think bananas, spinach, sweet potatoes, and beans. The DASH diet emphasizes these for proven pressure-lowering effects.
- Swap processed meats for grilled chicken or fish.
- Choose low-sodium soups or make your own with herbs.
- Opt for homemade pizza with veggies and minimal cheese.
- Reach for unsalted nuts or fresh veggies instead of chips.
- Select reduced-sodium cheese or smaller portions.
- Use lemon, vinegar, or spices in place of salty sauces.
- Limit pickled items or rinse them to cut sodium.
These changes align with heart-healthy patterns shown to reduce readings effectively.
Quick Comparison: Problem Foods vs. Better Choices
| Food to Limit | Typical Sodium per Serving | Main Concerns | Healthier Alternative | Benefit Highlight |
|---|---|---|---|---|
| Processed Meats | 500–1,000+ mg | High sodium + saturated fat | Fresh poultry or beans | Lower inflammation |
| Canned Soups | 800–1,200 mg | Extremely high sodium | Homemade or low-sodium versions | Better control |
| Pizza (Frozen/Restaurant) | 700–1,500 mg | Sodium + fats | Veggie-topped homemade thin crust | Reduced overall load |
| Salty Snacks | 150–300 mg | Easy to overeat sodium | Unsalted popcorn or carrots | Fewer empty calories |
| Cheese (Processed/Hard) | 300–500 mg | Sodium + saturated fat | Low-sodium varieties in moderation | Maintain flavor wisely |
| Condiments/Sauces | 200–900 mg | Hidden additions | Herbs, lemon, vinegar | Flavor without excess |
| Pickled Foods | 500–900 mg | Brine-heavy sodium | Fresh cucumbers or limited portions | Avoid fluid retention |
This side-by-side makes swaps clearer. Track portions for best results.

Practical Steps to Make Changes Stick
Read labels—choose items with 140 mg or less sodium per serving when possible. Cook more at home using fresh ingredients and spices. Rinse canned goods to slash sodium. Start by replacing one item weekly.
You might wonder, “Can I enjoy these occasionally?” Yes—moderation and balance matter. Occasional treats won’t derail progress if your overall pattern supports health.
Always consult your doctor or a dietitian before major shifts, especially with medications or conditions. They provide personalized guidance.
Take Control One Meal at a Time
Imagine steadier readings, more energy, and reduced worry about long-term risks. Ditching or limiting these seven foods empowers you toward better vascular health.
Your diet is a powerful tool. Which swap feels easiest to try first? Small steps lead to lasting change.
P.S. A quick home blood pressure check after meals reveals patterns—share trends with your healthcare provider for tailored support.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.