Imagine reaching for something on a high shelf, only to pause as your breath shortens unexpectedly, a subtle heaviness settling in your chest like an uninvited weight. That lingering tiredness after a simple walk, or the way your rings feel tighter some days—could these be everyday quirks, or whispers from a struggling heart? A weak heart, often linked to conditions like cardiomyopathy or heart failure, affects millions of Americans, quietly impacting daily life. In this article, we’ll uncover 10 common signs of a weakening heart and highlight 3 critical danger symptoms in heart failure that demand immediate attention. Envision the confidence of spotting these early, potentially opening doors to better management. But why do so many brush them aside?
A weak heart means reduced pumping efficiency, leading to symptoms that build gradually. The American Heart Association notes that recognizing signs early can support heart health significantly. Have you felt more winded than usual during routine tasks?
Dismissing these could allow progression, but awareness empowers action. Research suggests timely checks improve quality of life. What if that extra fatigue isn’t just aging?
These indicators often blend into busy lives, mistaken for stress or minor issues. Overlooking them might miss supportive interventions. Let’s start with the one that creeps in quietly.
These visuals illustrate common experiences with heart weakness.
Persistent Fatigue That Drains You
Picture Maria, 62, sinking into her couch earlier each evening, exhaustion wrapping around her like a heavy blanket despite restful nights. She thought it was work stress, but it deepened. Constant fatigue signals a weak heart struggling to circulate oxygen-rich blood.
Mayo Clinic highlights this as a primary sign in weakened cardiac function. That unrelenting tiredness, sapping your energy—could it be your heart?
But there’s more subtlety ahead. Ever feel breathless sooner?
Shortness of Breath on Exertion
Envision John, 65, huffing after climbing stairs, lungs burning faintly amid the familiar home scent. He blamed out-of-shape habits, yet it worsened with light activity. Dyspnea during effort indicates inefficient pumping.
Studies show this affects many with reduced heart strength. That quick winded feeling, air harder to catch—note it.
Hold on, swelling adds visibility. What about puffy changes?
Unexplained Swelling in Limbs
Recall Susan, 58, noticing ankles swollen by evening, skin shiny and indented from socks. She attributed it to standing, but it lingered. Edema from fluid retention points to backup in circulation.
Cleveland Clinic lists this commonly. That bloated heaviness, cool to touch—it’s telling.
Yet, chest discomfort lingers next. Ever sensed pressure?
Dull Chest Pain or Discomfort
Think of Robert, 70, feeling a vague ache while gardening, like a band tightening amid fresh earth smell. He dismissed indigestion, but it recurred. Chest unease can stem from strained heart muscle.
Sources note this in weakening hearts. That persistent pressure, warm and insistent—pay attention.
Intriguingly, palpitations disrupt rhythm. What if your heart flutters oddly?

Irregular or Rapid Heartbeats
Imagine Lisa, 60, sensing skips during quiet moments, heart racing unevenly like a misfiring engine. She ignored caffeine links, yet frequency rose. Arrhythmias often accompany reduced pumping.
Data links this to cardiac weakness. That fluttering thump, audible in silence—concerning?
But appetite wanes subtly. Ever feel full too soon?
Reduced Appetite and Nausea
Picture Tom, 67, leaving meals unfinished, stomach queasy despite favorite foods’ aroma. He thought diet changes, but nausea persisted. Digestive issues arise from congestion.
Research ties this to poor circulation. That early fullness, uncomfortable wave—observe it.
Surprisingly, dizziness strikes suddenly. What about lightheaded spells?
Frequent Dizziness or Lightheadedness
Envision David, 64, standing quickly, room spinning briefly, vision blurring in the haze. He blamed blood pressure, but repeats happened. Reduced blood flow to the brain causes this.
Guidelines mention it often. That unsteady sway, world tilting—alerting?
And weight fluctuates oddly. Ever gain pounds overnight?
:max_bytes(150000):strip_icc()/weak-heart-5184835-FINAL-edfc9bac6f404681a2b0a43b9228c5af.jpg)
Sudden Weight Gain
Recall Elena, 59, seeing the scale jump several pounds, clothes snugger without eating more. She puzzled, but fluid retention explained it. Rapid gain signals backup.
Tracking this is recommended. Those quick, heavy pounds—monitor closely.
Coughing irritates persistently. What if it’s more than a tickle?
Chronic Cough or Wheezing
Think of Mike, 68, coughing at night, wheezy with clear or pink mucus. He blamed allergies, yet it endured. Lung fluid from weak pumping triggers this.
Healthline reports it frequently. That stubborn hack, wet and tiring—listen.
Finally, activity tolerance drops. Ever limit your routines?
Decreased Exercise Tolerance
Imagine Patricia, 63, cutting walks short, fatigue hitting faster than before. She adapted gradually, but enjoyment faded. Lower stamina reflects overall weakness.
Multiple studies confirm this impact. That reduced endurance, frustratingly quick—it’s key.
These 10 signs—fatigue, shortness of breath, swelling, chest discomfort, palpitations, appetite loss, dizziness, weight gain, cough, and limited activity—can indicate a weakening heart.

Common heart failure symptoms visualized.
The 3 Danger Symptoms Demanding Urgent Care
In heart failure, some symptoms escalate to emergencies. Watch for these.
First, severe shortness of breath at rest or sudden worsening, especially with confusion—fluid overload can overwhelm quickly.
Second, intense chest pain radiating to arm, jaw, or back, often with sweating—this might signal acute crisis or attack.
Third, sudden fainting or severe dizziness with rapid pulse—indicating critical drop in output.
These require immediate medical help, like calling 911.

Warning signs of severe heart issues.
| Sign of Weak Heart | Common Misinterpretation | Potential Indicator |
|---|---|---|
| Persistent Fatigue | Busy lifestyle | Reduced oxygen delivery |
| Shortness of Breath | Lack of fitness | Inefficient pumping |
| Limb Swelling | Diet or standing | Fluid retention |
| Chest Discomfort | Stress or meals | Muscle strain |
| Palpitations | Anxiety | Arrhythmia |
| Appetite Loss | Stomach issues | Congestion |
| Dizziness | Dehydration | Low brain flow |
| Weight Gain | Eating habits | Fluid buildup |
| Chronic Cough | Cold or allergies | Lung fluid |
| Low Tolerance | Aging | Overall decline |
This helps distinguish patterns, but consult professionals.

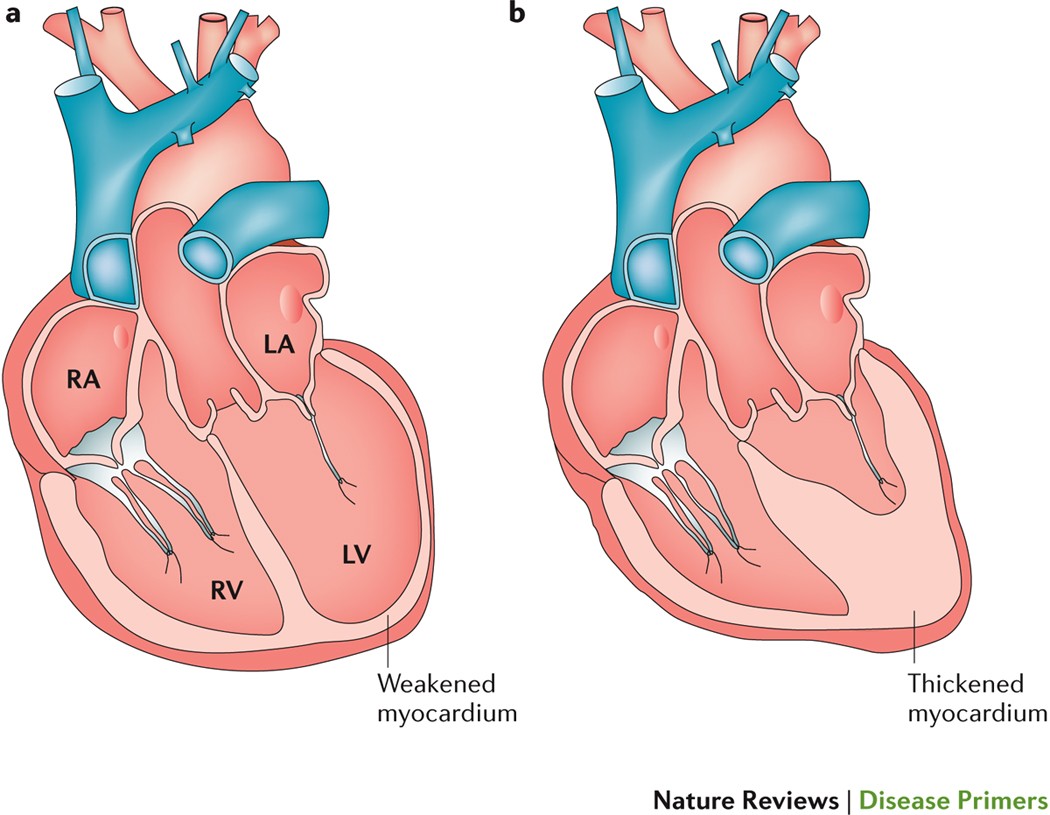
Comparison of normal vs. weakened heart.
Taking Proactive Steps Safely
If signs resonate, discussing with your doctor brings clarity. Tests like echoes provide insights. Take Anna, 66, facing fatigue and swelling. Before, fear loomed; after checks and guidance, she felt empowered, energy returning.
You might think, “It’s probably fine.” Many mimics exist, but evaluation reassures. Another: Frank, 69, ignored breath issues until danger signs—early talk shifted his path positively.
Always seek expert input.
| Step | Guidance | Notes |
|---|---|---|
| Symptom Journal | Record details daily | Aids accurate discussion |
| Provider Consultation | Share all observations | Include history |
| Tests if Suggested | BNP, echo, etc. | Informative, low risk |
| Lifestyle Talks | Activity, diet as approved | Personalized |
| Emergency Plan | Know danger signs | Act fast if needed |
These foster informed care.

Consulting a healthcare provider is essential.
Don’t overlook these signs or dangers—addressing them could unlock more vibrant years. Spotting fatigue, breath issues, and swelling, while heeding severe warnings, puts you in control. Imagine thriving with timely awareness.
P.S. A simple tip: Monitoring daily weight might catch fluid changes early, but discuss with your doctor first. Share this with loved ones—knowledge empowers everyone.
This article is for informational purposes only and is not a substitute for professional medical advice—readers are encouraged to consult their healthcare provider for personalized guidance.