Imagine sitting down to enjoy your favorite meal, only to feel that sharp, twisting pain return minutes later. Your stomach feels heavy, bloated, and inflamed—like it’s fighting against you. For those living with colitis, this isn’t just discomfort; it’s a daily struggle. And often, what triggers that pain is right there on your plate.
Colitis, whether ulcerative or inflammatory, can turn even healthy foods into hidden enemies. What’s tricky is that not every trigger is obvious—some are disguised as “gut-friendly” but can worsen inflammation quietly over time. Knowing which foods to avoid could help reduce flare-ups, calm your digestion, and help you reclaim control of your gut health.
So, what should you stay away from if you want fewer flare-ups and better gut comfort? Let’s uncover the 17 worst culprits—and what to eat instead.
Why Food Choices Matter in Colitis
Your colon is like a sensitive ecosystem. When inflammation hits, the lining becomes fragile, reacting strongly to anything that irritates it. Spicy meals, processed snacks, or even fiber-heavy foods can intensify that reaction.
You might think, “But I’m eating healthy!”—and you could be right. Yet, for someone with colitis, even raw vegetables or whole grains can cause irritation. The key isn’t eating less—it’s eating smarter.
When you understand which foods cause inflammation, bloating, or diarrhea, you can tailor your diet to support healing rather than sabotage it.
Let’s start with the top triggers.
1. Dairy Products
Lisa, 42, loved her morning latte—until she noticed every cup brought cramps and urgency. Dairy contains lactose, which many people with colitis struggle to digest. When lactose lingers in the gut, it ferments, leading to gas and irritation.
Try switching to lactose-free milk, almond milk, or oat milk instead. They’re gentler and just as satisfying.
2. High-Fat Fried Foods
Greasy fries, fried chicken, or doughnuts may look tempting, but they can cause chaos in your gut. Fat slows digestion, forcing your inflamed colon to work harder.
Instead, try air-fried or baked versions. Your taste buds won’t notice much difference—but your colon will.
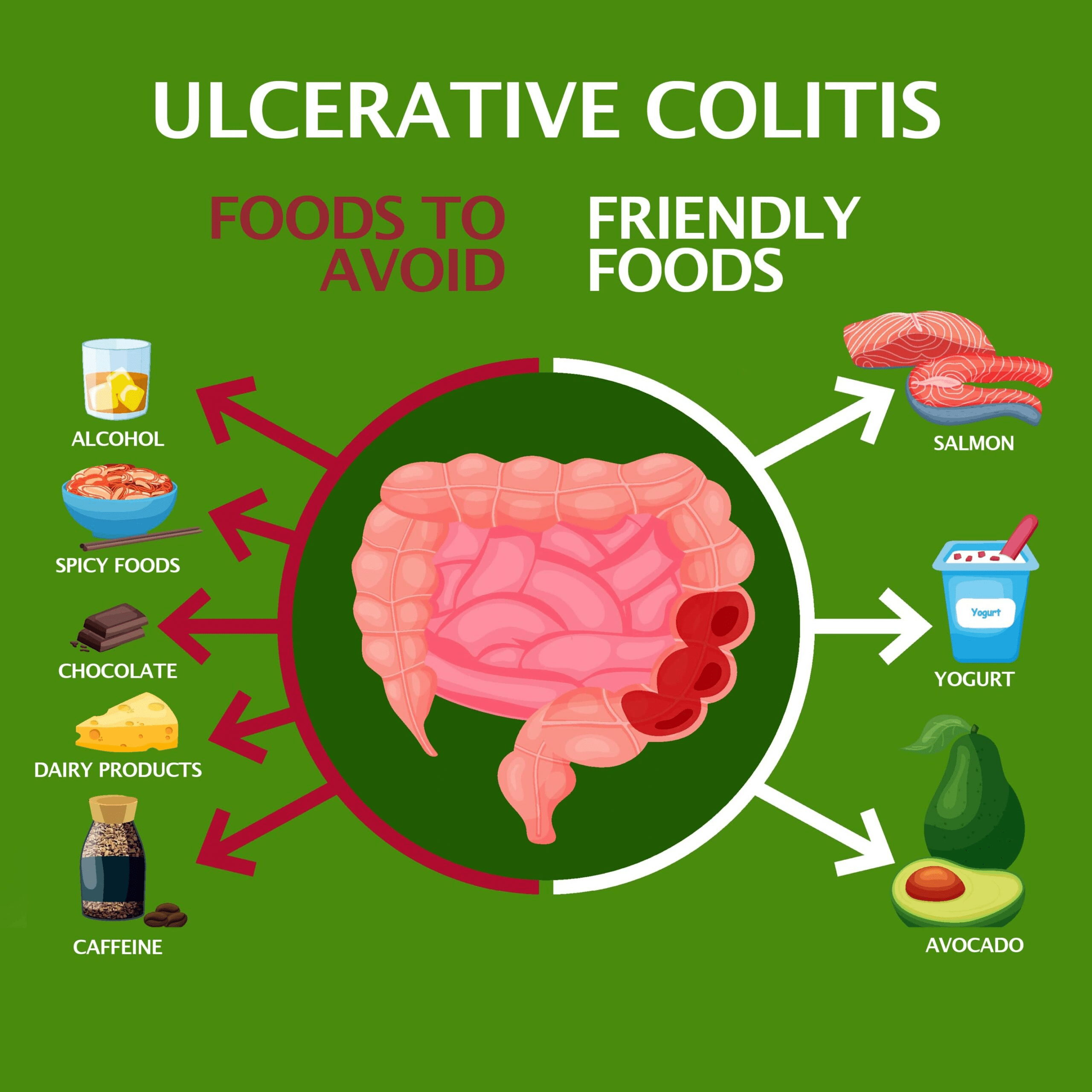
3. Caffeine
Coffee lovers, this one’s tough. Caffeine stimulates bowel movements, which can trigger diarrhea during flare-ups. It also increases acidity, worsening pain.
If you can’t give it up completely, limit yourself to one cup or switch to herbal teas like chamomile or peppermint.
4. Alcohol
That evening glass of wine might feel relaxing, but alcohol can irritate your colon lining, leading to dehydration and inflammation. Even small amounts may spark discomfort.
Opt for mocktails or sparkling water with lemon—refreshing and gut-friendly.
5. Carbonated Drinks
Soda and fizzy drinks introduce excess air into your digestive tract, leading to bloating and pressure. For someone with colitis, that discomfort can escalate quickly.
Choose still water or fresh juice instead—it’s kinder to your system.
6. Red Meat
Red meat is rich in fat and protein that can be difficult for your inflamed colon to process. Research suggests it may contribute to flare-ups.
If you crave protein, go for fish or skinless poultry. They’re easier to digest and less inflammatory.
7. Spicy Foods
Chili, hot sauce, and spicy curries might add flavor—but they can also inflame your gut. Capsaicin, the active compound in peppers, irritates the colon lining.
Try seasoning with herbs like basil, parsley, or turmeric for a flavorful, gentle alternative.
8. Raw Vegetables
Raw veggies are packed with fiber—but that’s exactly the problem. For a sensitive colon, roughage can be harsh and cause bloating or cramps.
Steam or roast your vegetables instead. They’ll retain nutrients but be much easier to digest.
9. Whole Nuts and Seeds
Nuts and seeds are healthy fats, but their hard texture can scrape the intestinal wall during flare-ups. They also move through the gut slowly, prolonging discomfort.
Try smooth nut butters or seedless spreads to enjoy the taste without the irritation.
10. Popcorn
Popcorn is a classic movie-night snack—but for colitis sufferers, those tough kernels are bad news. They’re hard to digest and can get trapped in inflamed tissue.
Soft snacks like rice cakes or baked apple slices make a safer alternative.
11. Corn and Corn-Based Products
Corn’s outer shell contains cellulose, a fiber the human gut can’t fully digest. It often leads to bloating and cramping in those with colitis.
Replace corn with mashed potatoes or pureed vegetables for comfort and ease.
12. Beans and Lentils
Though rich in protein, beans contain oligosaccharides—sugars that cause gas. During a flare-up, that gas can feel like pressure and pain.
If you enjoy legumes, try pureed lentil soups or small portions in remission phases.

13. Gluten-Containing Grains
For some, gluten can exacerbate inflammation and trigger immune responses. Wheat, barley, and rye are common culprits.
Opt for gluten-free grains like rice, quinoa, or oats to reduce irritation.
14. Processed Foods
Anything boxed, packaged, or full of preservatives often contains additives and refined oils that aggravate the colon.
Focus on whole foods—fresh fruits, lean proteins, and simple grains—to keep digestion calm and predictable.
15. Artificial Sweeteners
Sugar-free gum and diet sodas might sound harmless, but sweeteners like sorbitol or sucralose can cause bloating and diarrhea.
Choose natural sweeteners like honey or maple syrup in moderation.
16. Onions and Garlic
They’re kitchen staples, but onions and garlic contain fructans—carbs that ferment quickly in the gut, causing gas and bloating.
Try cooking them thoroughly or using infused oils for a milder flavor without the harsh effects.
17. Cruciferous Vegetables
Broccoli, cauliflower, and cabbage are nutrient-rich but gassy. Their sulfur compounds can worsen cramps and bloating.
During remission, introduce small amounts slowly, cooked until soft.
Now that we’ve covered what to avoid, let’s explore what you can do to soothe your gut instead.
The Balanced Way Forward
Avoiding trigger foods doesn’t mean eating blandly—it’s about creating comfort in every bite. When your gut is inflamed, gentle nutrition can make all the difference.
| Food Type | Better Choices | Why It Helps |
|---|---|---|
| Grains | White rice, oatmeal | Easy to digest and low residue |
| Protein | Fish, eggs, tofu | Gentle on the gut |
| Vegetables | Cooked carrots, pumpkin, zucchini | Soft texture, low fiber |
| Fruits | Bananas, applesauce | Soothing and nutrient-rich |
And here’s another tip: keep a food journal. Write down what you eat and how your body reacts. Over time, you’ll discover your personal triggers and safe foods.

Real-Life Insight: A Gut Comeback
Mark, 51, battled ulcerative colitis for years. “Every meal was a gamble,” he said. After eliminating red meat, soda, and dairy, and focusing on cooked vegetables and fish, his energy returned. “I still have bad days,” he admitted, “but now I know how to stop them before they spiral.”
Food became his medicine—not through restriction, but through awareness.
The Golden Tip: Listen to Your Gut
Your digestive system speaks; you just have to listen. When something feels off, it’s a message. Avoiding these 17 foods may help calm inflammation, reduce symptoms, and give your colon the break it deserves.
Remember, everyone’s colitis journey is unique. What irritates one person may not affect another. The key is mindful eating—tuning in, adjusting, and nourishing yourself with patience.
Imagine enjoying meals again without fear of flare-ups. It starts with one choice, one plate, one mindful moment.
Your gut wants balance—and with the right foods, you can give it exactly that.
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider for personalized guidance.