Imagine noticing a small change in your body—something subtle, easy to brush off as stress, age, or just “one of those things.” For many women, that’s exactly how cervical cancer starts: quietly. This slow-growing disease often shows no obvious signs in its earliest, most treatable stages. Yet when symptoms do appear, they can signal that the cancer has begun to advance. The good news? Regular screenings catch issues long before symptoms ever show up.
Have you ever wondered if you’re paying enough attention to your body’s signals? Cervical cancer remains one of the few cancers we can largely prevent and detect early. Let’s explore what science tells us about the signs worth noticing—and why acting promptly matters.
Why Cervical Cancer Can Stay Silent for So Long
Cervical cancer begins in the cells of the cervix, the lower part of the uterus that connects to the vagina. Nearly all cases link to persistent infection with high-risk strains of human papillomavirus (HPV), a very common sexually transmitted virus.
In early stages—or even with precancerous changes—most women experience no symptoms at all. This silent phase can last years. That’s why reliable sources like the Mayo Clinic, American Cancer Society, and CDC emphasize that symptoms usually emerge only when the cancer grows larger or spreads to nearby tissues.
Ignoring subtle changes risks allowing the disease to progress. But recognizing them early gives you power. Ready to learn the key signs most often mentioned by medical experts?
Countdown: 9 Important Signs to Watch For
Here are nine changes that may point to cervical cancer, especially when they persist or feel unusual for you. Remember, these can stem from many non-cancer causes too—but they deserve a doctor’s attention.
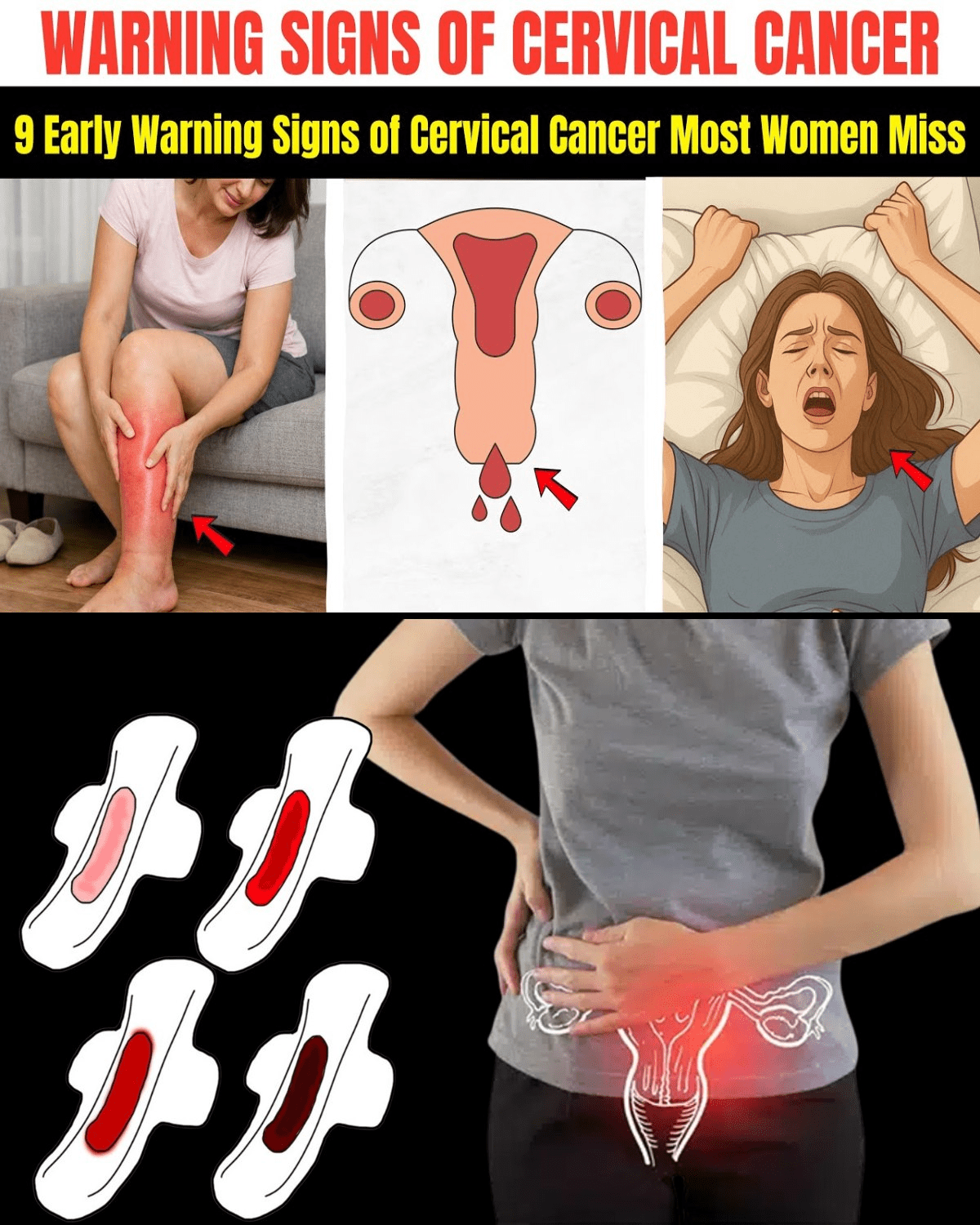
9. Unusual Vaginal Discharge A watery, bloody, or pinkish discharge that appears between periods or after menopause often raises concern. Sometimes it carries a foul odor. Many women first notice this as a persistent change in their normal pattern.
8. Abnormal Vaginal Bleeding Bleeding after intercourse, between menstrual periods, after menopause, or periods that suddenly become heavier or last much longer than usual. This ranks among the most commonly reported early indicators.
Here’s a visual of what abnormal bleeding might look like on a pad—something many women spot first.


7. Pain During Intercourse New or increasing discomfort during sex can occur as the tumor affects nearby tissues. If intimacy has become painful when it wasn’t before, don’t dismiss it.
6. Pelvic Pain or Pressure A dull, persistent ache or feeling of heaviness in the lower abdomen or pelvis. This may feel like constant period cramps outside your cycle.
Many women describe this sensation clearly.

Pelvic Health Q&A – Spooner Health
5. Leg Pain or Swelling In more advanced cases, swelling in one or both legs or pain that feels like a deep ache. This happens when swollen lymph nodes or tumor growth affects blood flow.
4. Lower Back Pain Ongoing lower back discomfort that doesn’t respond to usual remedies. Sometimes cancer pressing on nearby structures causes this.
3. Urinary or Bowel Changes Difficulty urinating, blood in urine, frequent urination, or bowel changes like constipation. These appear when the cancer impacts the bladder or rectum.
2. Unexplained Fatigue and Weight Loss Feeling unusually tired or noticing unintentional weight loss. These general symptoms often show up in later stages.
1. The Silent Precursor: No Symptoms at All The most important “sign” is actually the absence of any—because early cervical cancer and precancers rarely cause noticeable changes. This makes regular screening the true lifesaver.
But wait—there’s something even more powerful than watching for symptoms.
Real Stories of Women Who Acted Early
Take Emily, 42, who noticed light spotting after exercise. She thought it was hormonal. A quick doctor’s visit led to an abnormal Pap result, early detection, and successful treatment. “I almost ignored it,” she says. “That small sign saved me.”
Or Sarah, 38, who experienced pain during intimacy for months before mentioning it. Her gynecologist found precancerous cells. Simple treatment followed. Today she encourages every woman: “If something feels off, speak up.”
Could a routine check make the same difference for you?
The Real Key to Protection: Prevention and Screening
The best defense isn’t waiting for symptoms—it’s preventing the disease entirely.
- Get the HPV vaccine if eligible (ideally before sexual activity, but catch-up options exist up to certain ages).
- Schedule regular screenings. Current guidelines (as of 2025) recommend:
- Ages 25–65: Primary HPV test every 5 years (preferred), or co-testing (HPV + Pap) every 5 years, or Pap alone every 3 years.
- New option: Self-collection for HPV testing in many settings—more convenient than ever.
- Practice safe sex and avoid smoking (it worsens HPV persistence).
Here’s a clear diagram of the female reproductive system to help visualize where cervical cancer starts.
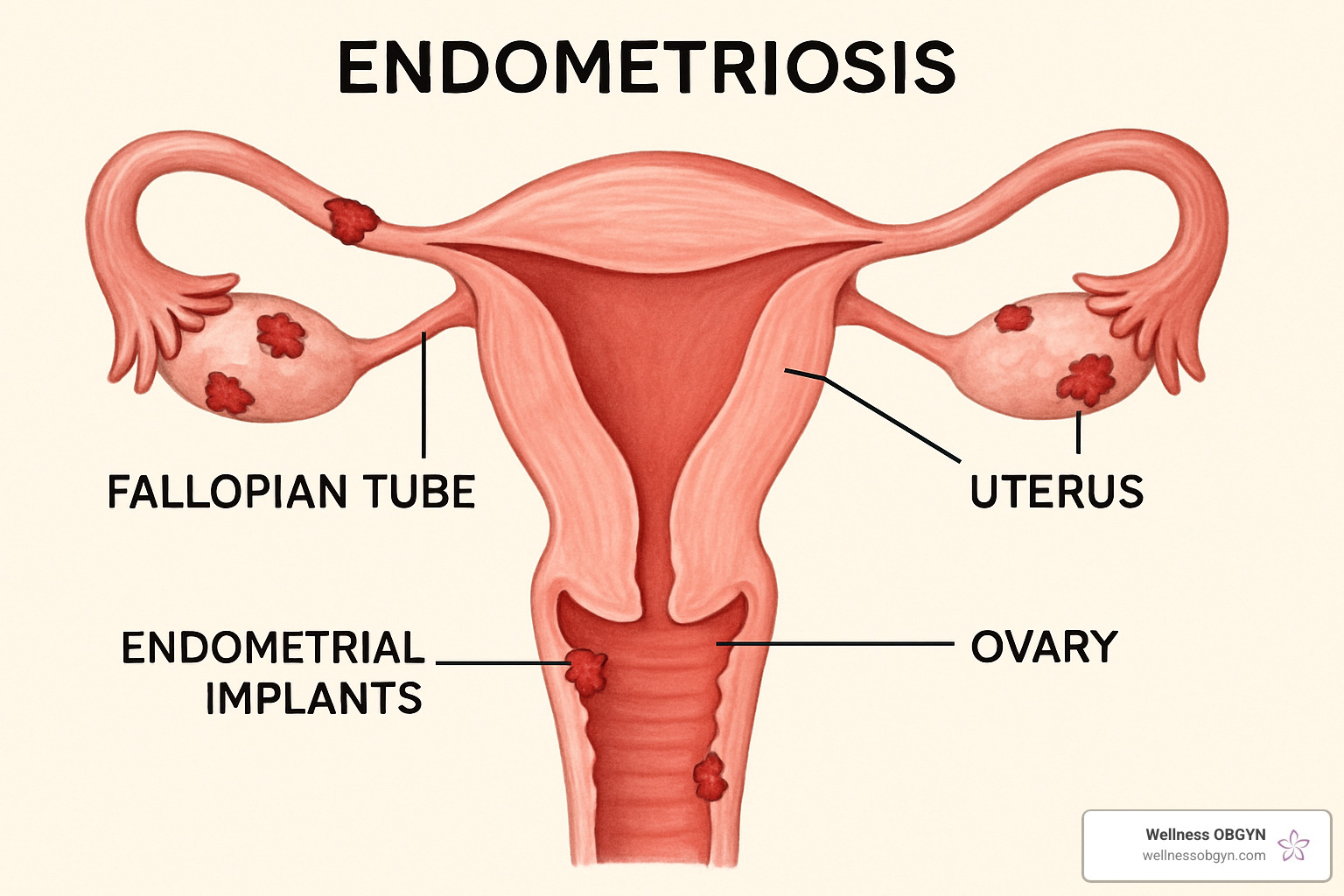
Honolulu Women’s Health: Wellness OBGYN (2025)
Quick Comparison: Early vs. Advanced Signs
| Stage | Typical Signs | Action Needed |
|---|---|---|
| Early/Precancer | Usually none | Routine screening detects it |
| Early Invasive | Abnormal bleeding, unusual discharge, pain during sex | See doctor promptly |
| Advanced | Pelvic/back pain, leg swelling, urinary/bowel issues | Urgent medical evaluation |
Take the First Step Toward Peace of Mind
What if you scheduled that overdue screening this month? Many women discover everything is fine—and those who find something early often face straightforward solutions.
You deserve to feel confident about your health. Listen to your body, but don’t rely on symptoms alone. Talk to your healthcare provider about your screening schedule, especially if you’re between 25 and 65.
Share this with a sister, friend, or daughter. One conversation can spark life-changing action.
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider if you have any concerns about your health or symptoms. Cervical cancer screening and prevention recommendations may vary based on individual risk factors—discuss your personal plan with a qualified professional. Individual results and experiences vary.