You wake up one morning feeling unusually tired. Your chest feels tight, your breath shorter than usual. You blame stress, maybe your age, or even last night’s heavy dinner. But deep down, something doesn’t feel right. What if these small, quiet changes are your body’s early warning signs of a heart attack?

Every year, hundreds of thousands of people experience heart attacks — many without realizing their body had been sending signals for weeks. These symptoms don’t appear overnight. They build slowly, like whispers from your heart begging to be heard.
The truth is, heart attacks rarely strike “out of the blue.” Your body often gives you a 30-day window of opportunity to act — if you know how to read the signs.
Let’s uncover the 7 early symptoms that can appear up to a month before a heart attack, what they really mean, and how you can respond before it’s too late.
Why Early Detection Matters
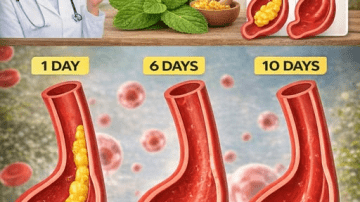
The heart is a tireless worker, beating around 100,000 times a day to pump blood through 60,000 miles of vessels. But when those vessels narrow or clog with plaque, your heart struggles to get oxygen — that’s when danger begins.
In the weeks before a heart attack, blood flow may already be restricted. Your body tries to compensate, producing small but noticeable symptoms. The earlier you notice these, the more time you have to protect your heart and possibly prevent a major event.
So, what should you look for? Let’s start with one of the most common — but misunderstood — early signs.
1. Unusual Fatigue That Doesn’t Go Away
Have you felt drained lately, even after sleeping well? Many people — especially women — report persistent, unexplained fatigue in the weeks before a heart attack.
Margaret, 62, said, “I felt like I was walking through wet sand every day. Even grocery shopping wore me out.”
This fatigue happens because your heart struggles to pump enough oxygen-rich blood to your muscles and brain. It’s not just tiredness; it’s your body working overtime to compensate for reduced circulation.
You may notice it most during simple tasks — climbing stairs, carrying groceries, or even getting dressed.
And if you think rest will fix it, think again. Fatigue from a struggling heart doesn’t fade after a nap.
But fatigue isn’t the only sign hiding in plain sight…
2. Shortness of Breath — Even at Rest
If you find yourself gasping for air during light activity, or waking up short of breath at night, it could mean fluid is building up in your lungs due to poor heart function.
When the heart can’t pump efficiently, blood backs up into the lungs, causing breathlessness — a key warning sign.
Paul, 68, recalls, “I used to mow the lawn without stopping. Suddenly, I had to pause every few minutes just to catch my breath.”
You might notice this especially when lying flat or walking uphill. Some people mistake it for asthma or lack of fitness, but if it’s new or persistent, your heart could be the real cause.
And there’s another symptom that might show up in your body before you feel it in your chest…
3. Chest Pressure or Discomfort
When people imagine a heart attack, they think of sharp pain. But early heart distress often feels different — a dull pressure, fullness, or heaviness in the center or left side of the chest.
It can last a few minutes, fade, then return. You might describe it as tightness, burning, or an “elephant sitting on your chest.”
This sensation means your heart muscle isn’t getting enough oxygen. Don’t dismiss it as heartburn or indigestion, especially if it occurs with exertion or stress.
Sometimes, the discomfort spreads — which brings us to the next warning sign.

4. Pain in the Jaw, Neck, or Shoulder
Your heart and body share the same network of nerves, which means pain can radiate to unexpected places. Some people feel discomfort in their jaw, neck, shoulder, or upper back instead of the chest.
David, 59, first noticed stiffness in his left shoulder while driving. “I thought I’d slept wrong,” he said. “A month later, I had a mild heart attack.”
This referred pain often appears during activity and fades at rest — another key clue it’s heart-related, not muscular.
And if the pain starts spreading downward… take note.
5. Arm or Upper Back Discomfort
A heavy, tingling, or numb feeling in one or both arms — especially the left — can appear days or weeks before a heart attack. Some describe it as “pins and needles,” others as dull soreness that comes and goes.
This happens because reduced blood flow affects nerve pathways leading from the heart. The discomfort can even extend to your upper back, between the shoulder blades.
It’s not always severe — sometimes it’s just different. If it feels unfamiliar or persistent, don’t wait for it to worsen.
But one of the earliest warnings comes not from pain… but from your gut.
6. Indigestion, Nausea, or Stomach Discomfort
Many people mistake heart-related symptoms for digestive issues. You might feel bloated, queasy, or experience mild stomach pain — particularly after eating.
This happens when reduced blood flow triggers signals in the vagus nerve, which connects the heart and stomach.
Nancy, 71, recalled, “I felt like I had heartburn for weeks. Antacids didn’t help. It turned out my heart was the problem, not my stomach.”
If you notice persistent nausea or pressure after meals — especially when paired with fatigue or breathlessness — it could be a subtle sign of heart strain.
And there’s one final symptom that often appears just before serious trouble begins…
7. Lightheadedness, Dizziness, or Cold Sweats
Have you ever felt suddenly dizzy, clammy, or weak without explanation? These sensations can occur when blood pressure drops due to a struggling heart.
Your brain gets less oxygen, causing lightheadedness or even brief fainting. The body may respond by producing cold sweats as it tries to rebalance blood flow.
You might feel like you’re coming down with the flu, but this “flu” doesn’t go away. It’s your body’s distress signal — one that shouldn’t be ignored.
Here’s a summary of these key warning signs:
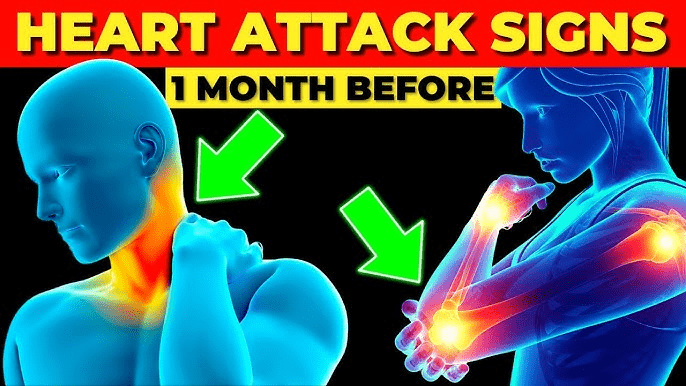
Table: Early Symptoms of Heart Attack (Up to One Month Before)
| Symptom | What It Means | When to Act |
|---|---|---|
| Unusual fatigue | Low oxygen supply | If persistent for days |
| Shortness of breath | Fluid buildup in lungs | If frequent or worsening |
| Chest pressure | Reduced blood flow | If recurring |
| Jaw/neck/shoulder pain | Referred nerve pain | If during activity |
| Arm or back discomfort | Circulatory restriction | If recurring |
| Indigestion/nausea | Nerve-related heart distress | If lasting >1 week |
| Dizziness/cold sweats | Drop in circulation | Immediate check-up |
But recognizing the symptoms is only half the battle — the next step is knowing how to respond.
What to Do If You Notice These Symptoms
- Don’t wait it out. If symptoms persist or come in patterns, schedule a medical evaluation. Early testing can detect narrowed arteries before a crisis occurs.
- Track your symptoms. Note when they occur — during activity, rest, or stress — and how long they last. This helps doctors identify underlying causes.
- Adopt heart-supportive habits.
- Eat more fruits, vegetables, and whole grains.
- Reduce sodium and processed foods.
- Stay active but avoid overexertion.
- Manage stress with deep breathing or meditation.
- Seek emergency care if symptoms suddenly worsen — particularly chest pain, severe breathlessness, or collapse.
And if you’re wondering, “Can these signs appear a full month in advance?” — yes. Research shows many heart attack survivors experienced at least one warning sign in the 30 days prior. The key difference between survival and tragedy often lies in how soon they recognized and acted.
Real-Life Story: A Wake-Up Call
Ron, 65, had been feeling tired for weeks. He blamed his busy schedule. Then came the shortness of breath climbing stairs. “It wasn’t painful — just strange,” he said. His wife insisted he see a doctor. Tests revealed significant blockage in two arteries.
After treatment and lifestyle changes, Ron says, “I learned to listen to my body. It was trying to save me.”
Your body does the same — but you have to pay attention before those whispers become alarms.
How to Protect Your Heart Starting Today
| Step | Action | Why It Matters |
|---|---|---|
| 1 | Get a heart screening | Detects risk early |
| 2 | Control blood pressure & cholesterol | Reduces strain on arteries |
| 3 | Exercise moderately | Strengthens heart muscle |
| 4 | Eat smart | Improves circulation |
| 5 | Manage stress | Lowers cortisol & heart load |
Small daily actions — like a 20-minute walk, deep breathing before bed, or swapping fried foods for grilled — can lower your risk more than you might imagine.
The Bottom Line: Listen Before It’s Too Late
A heart attack rarely starts with collapse — it starts with whispers. Fatigue, shortness of breath, chest pressure — these are your early alerts. Ignoring them could mean missing your best chance to prevent disaster.
So if your body feels “off,” don’t dismiss it as age or stress. Pause. Listen. Act.
Your heart has been beating faithfully for you every second of your life — maybe now it’s time you return the favor.
This article is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider for personalized guidance.