You probably take medicine to feel better—to ease pain, fight infections, or help you sleep. But what if the very pills you trust could be quietly damaging one of your body’s most vital organs? Imagine waking up one morning with unexplained fatigue, yellowing eyes, or a dull ache under your ribs—only to discover your liver has been struggling in silence for months.
It sounds dramatic, but liver damage often creeps in without obvious pain. And here’s the unsettling part: some of the most common medications in America—the ones millions take daily—can contribute to liver injury when used improperly or even at normal doses for too long.
So, which ones are the real culprits? How do you recognize the danger before it’s too late? And most importantly—what can you do to protect your liver without giving up the medications you need?
Let’s peel back the curtain and uncover what doctors rarely tell you about everyday drugs and your liver health.
The Hidden Crisis: How Medications Attack the Liver
Your liver is the ultimate multitasker—it filters blood, detoxifies chemicals, and processes every medication you swallow. But this hero organ has a limit. When it’s overloaded with certain drugs or combinations, the result can be inflammation, scarring, and eventually liver failure.
Here’s the twist: most people don’t feel anything until serious damage has occurred. By the time fatigue, nausea, or yellowing skin appear, the liver may already be in distress.
The scary part? Some of these medications are likely sitting in your medicine cabinet right now.

The Countdown: 10 Medications That May Harm Your Liver
Let’s walk through the top 10 offenders—starting with the most surprising ones.
10. Acetaminophen (Tylenol)
Sarah, a 47-year-old teacher, used Tylenol daily for headaches. She followed the label—most days. But over time, her liver enzymes spiked.
Acetaminophen is one of the leading causes of acute liver failure in the U.S. Taking more than 3,000–4,000 mg per day—or combining it with alcohol—can be dangerous.
Hint: Even “cold and flu” or “pain relief” combos often hide acetaminophen inside.
Think you’re safe because you don’t drink alcohol? Think again—the risk builds quietly over time.
9. Statins (for Cholesterol)
You’ve heard statins save lives by lowering cholesterol—but they also make your liver work overtime. Most people tolerate them well, but for some, they can cause enzyme elevations that signal stress.
You might feel fine… until your routine blood test says otherwise.
Watch for: fatigue, dark urine, or unexplained muscle pain.
But wait—there’s a twist: stopping statins without medical guidance can be riskier for your heart. Always check with your doctor before making changes.
8. Certain Antibiotics
Some antibiotics—like amoxicillin-clavulanate, erythromycin, and tetracycline—can lead to liver inflammation or bile obstruction.
Tom, 56, was prescribed an antibiotic for sinusitis. Two weeks later, he noticed yellow eyes and itchy skin. His diagnosis? Drug-induced hepatitis.
Pro tip: ask your doctor if your antibiotic has known liver risks—especially if you have pre-existing conditions.
7. Anti-Seizure Drugs (Phenytoin, Valproate, Carbamazepine)
These powerful medications help control seizures but can trigger enzyme spikes or, rarely, liver failure—particularly in the first few months of treatment.
If you’ve ever noticed fatigue or abdominal tenderness while taking them, don’t dismiss it.
Here’s a surprise: some herbal “calming” supplements may worsen the effect when combined with anti-seizure drugs.
6. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Ibuprofen, naproxen, and diclofenac relieve pain—but long-term or high-dose use can inflame the liver.
Ever wonder why your doctor says “take with food”? It’s not just about the stomach—your liver also feels the impact.
A quick check: do you combine painkillers with alcohol on weekends? That’s a double hit your liver won’t thank you for.
5. Antifungal Medications (Ketoconazole, Itraconazole)
They fight stubborn infections but can block liver enzymes responsible for detox.
You might not feel symptoms right away—but your blood tests could show elevated ALT or AST levels.
Here’s something few mention: topical antifungals (like creams) are usually much safer than pills.
4. Methotrexate (for Arthritis and Cancer)
Methotrexate helps millions manage inflammation and cancer. Yet over time, it may scar the liver—especially if combined with alcohol or other drugs.
Doctors usually order regular liver tests for this very reason.
Still, many people skip checkups, thinking “I feel fine.” That’s where trouble begins.
3. Antidepressants (SSRIs and Tricyclics)
Yes, even medications meant to lift your mood can put your liver to work. Fluoxetine (Prozac), sertraline (Zoloft), and amitriptyline are among those linked to mild liver stress.
For most, it’s reversible—but for some, enzyme spikes persist.
Could your fatigue or digestive issues be more than just stress? It might be worth asking your doctor about a liver test.
2. Anabolic Steroids
Used medically for hormone disorders—or illicitly for muscle gain—these compounds can block bile flow and cause jaundice.
Even “natural” performance boosters sometimes contain hidden steroids.
Quick thought: if a supplement promises fast muscle growth, there’s a good chance your liver pays the price.
1. Herbal and Over-the-Counter “Detox” Supplements
Ironically, the products marketed to cleanse your liver can sometimes do the opposite.
Supplements containing green tea extract, kava, or comfrey have been linked to liver injury.
The shocking truth: “natural” doesn’t always mean “safe.”
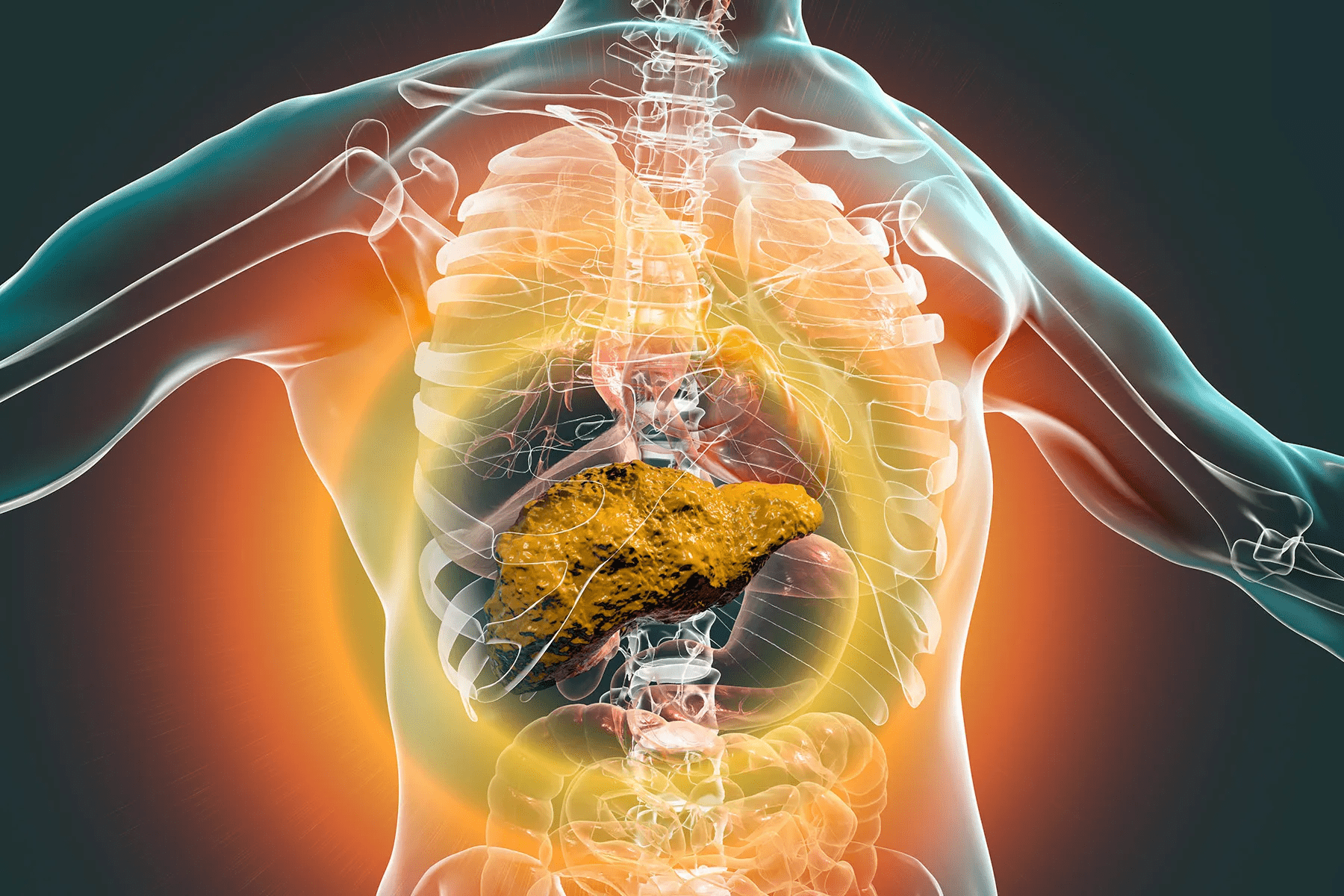
Early Signs Your Liver Might Be in Trouble
Your liver doesn’t cry out in pain—it whispers. Here’s what it might be trying to tell you:
- Fatigue that doesn’t go away with rest
- Yellowish skin or eyes (jaundice)
- Itchy skin or dark urine
- Loss of appetite or nausea
- Pain or pressure under your right ribs
If you’ve noticed even one of these symptoms and take medications regularly, it may be time for a checkup.
Table 1: Comparing Medication Impact on Liver
| Category | Common Examples | Potential Liver Effect | Monitoring Needed |
|---|---|---|---|
| Pain Relief | Acetaminophen, NSAIDs | Enzyme elevation, acute injury | Regular blood tests |
| Cholesterol | Statins | Mild to moderate enzyme rise | Periodic liver panel |
| Mental Health | SSRIs, TCAs | Mild enzyme stress | Baseline test |
| Infections | Antibiotics, Antifungals | Inflammation, bile obstruction | During treatment |
| Chronic Illness | Methotrexate | Long-term scarring risk | Every 2–3 months |
Protecting Your Liver: Smart, Safe Steps
So what can you actually do without giving up your meds?
- Follow dosage precisely. More isn’t better—especially for painkillers.
- Avoid mixing alcohol and medication. Even a glass of wine can increase risk.
- Get routine blood tests. Especially if you take long-term prescriptions.
- Ask before mixing drugs or supplements. Some “natural” remedies aren’t harmless.
- Stay hydrated and eat liver-friendly foods. Think leafy greens, turmeric, and garlic.
Table 2: Safe Use Guidelines
| Medication Type | Safer Practice | When to Call Your Doctor |
|---|---|---|
| Painkillers | Max 3,000 mg/day acetaminophen | Yellow eyes, dark urine |
| Statins | Avoid alcohol, test every 6 months | Muscle pain or fatigue |
| Antidepressants | Take with food, monitor mood and digestion | Persistent nausea |
| Antibiotics | Complete full course, hydrate | Rash, jaundice |
| Supplements | Check for third-party testing | Any abnormal symptoms |
Two Real Stories, One Lesson
Case 1: Sarah, 47
After months of daily Tylenol for migraines, Sarah began feeling exhausted and bloated. A simple blood test revealed elevated liver enzymes. Once she reduced dosage and added liver-friendly foods, her numbers normalized within months.
Case 2: Tom, 56
Tom’s antibiotic treatment triggered severe itching and yellow eyes. Early detection saved him from lasting damage. Today, he reads every medication label—and so should you.

Could This Be Happening to You?
Take a quick self-check:
- Do you take more than one medication daily?
- Have you skipped liver tests because you “feel fine”?
- Do you occasionally mix meds with alcohol?
If you answered “yes” to even one, your liver might deserve more attention.
The Takeaway: Your Liver Can Heal—If You Act Early
The good news? The liver is remarkably resilient. Many cases of drug-related damage can reverse once the cause is identified and removed.
So, don’t panic—get proactive. Talk with your healthcare provider, schedule that overdue blood test, and make small lifestyle adjustments today.
Because when your liver thrives, your whole body feels it—energy returns, digestion improves, and clarity follows.
P.S. Did you know your liver regenerates itself faster than almost any other organ? But it can only do that if you give it a break.
So share this with someone who might need it—you never know whose health you could save.
This article is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider for personalized guidance.